Can Personalised Nutrition Interventions Be Used To Support Long Haul Covid?
- Rachel Jessey

- Feb 28, 2022
- 7 min read
Updated: Nov 1, 2023
What is Long Haul Covid?

Several people might be left with long-term symptoms of an infection caused by Covid-19, even though the initial phase passes quickly. These symptoms have collectively been referred to as Long Covid. While there are some differences in definitions across health care authorities, the NICE guidelines and the CDC define long-term Covid patients as those with ongoing symptoms that persist beyond four weeks from initial infection. (1)
Official definitions from NICE:
Acute COVID-19 Signs and symptoms of COVID‑19 for up to 4 weeks. Ongoing symptomatic COVID-19 Signs and symptoms of COVID‑19 from 4 weeks up to 12 weeks. Post-COVID-19 syndrome Signs and symptoms that develop during or after an infection consistent with COVID‑19, continue for more than 12 weeks and are not explained by an alternative diagnosis. In addition to the clinical case definitions, the term ‘long COVID’ is commonly used to describe signs and symptoms that continue or develop after acute COVID‑19. It includes both ongoing symptomatic COVID‑19 (from 4 to 12 weeks) and post‑COVID‑19 syndrome (12 weeks or more). (2)
It is believed that Long Covid is caused by immune system alterations secondary to an initial infection. This causes chronic low-grade inflammation with or without increased histamine release, and increased blood clotting. (5)
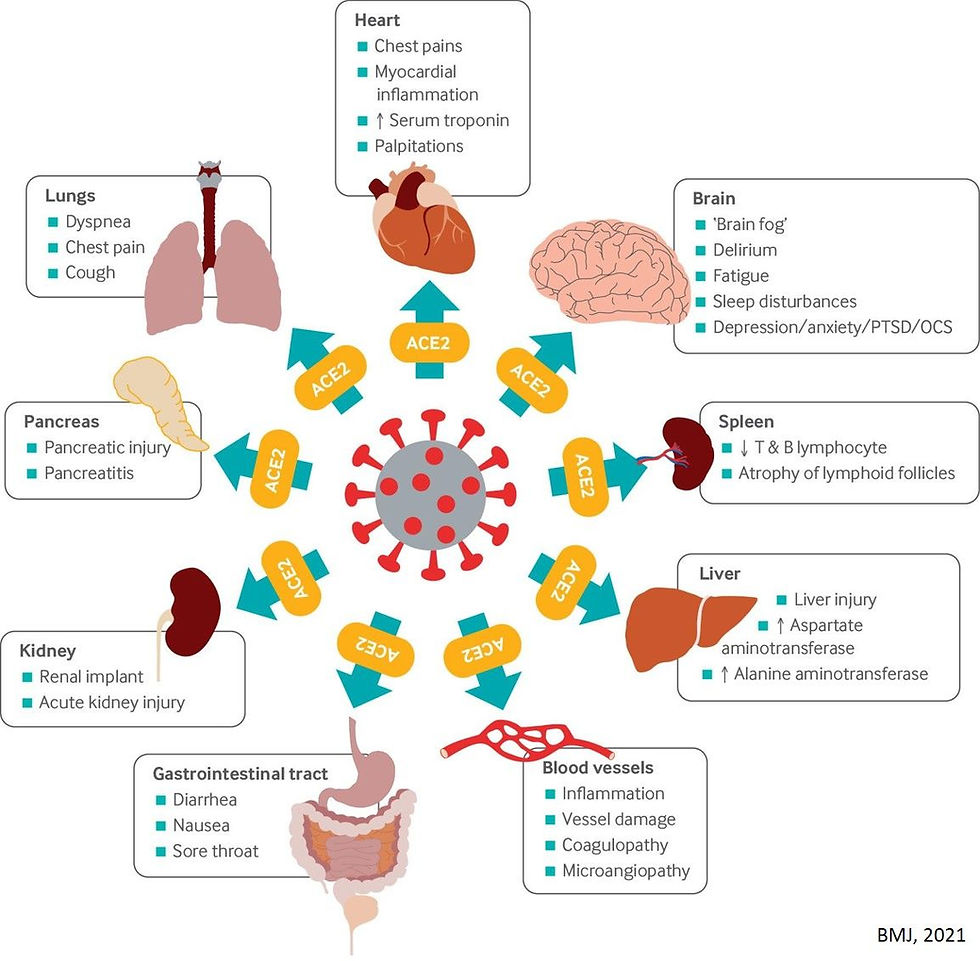
Individuals with Long Covid may experience clusters of symptoms, often overlapping, fluctuating and changing over time. The symptoms can range from mild to debilitating and may last for several weeks to months. In addition to the severity of the initial infection, previous comorbidities may affect how severe Long Covid symptoms will be (3). As described within an article in the British Medical Journal, the ACE2 receptors, which the virus uses to gain entry into the cells, are located in multiple areas of the human body. This includes the lungs, gut, heart, brain, and blood vessels and explains why symptoms can appear in many areas. (1). Fatigue, shortness of breath and joint pain appear to be the most reported symptoms and at this present time it is not known if vaccines have any effect on ongoing symptomatic Covid-19 or the prevention of Long Covid. (2)
Nutritional Therapy Strategies for Long Haul Covid
Targeted therapy
Although the research is still ongoing, it is generally accepted that targeted nutritional therapy to support recovery from Covid-19 infection should be started as early into the illness and sustained throughout the recovery period if health outcomes are to be optimised. The impact of inadequate nutrition throughout these stages not only increases the risk of nutritional deficiencies but may extend recovery time. (4)
Proposed Nutritional Therapy Model
Once a patient recovers from the acute phase of illness and depending on individual health outcomes, the following strategies can be adopted:
Patients should have access to a multi-disciplinary team, based on the individual needs and goals identified during a thorough nutritional assessment
Patients should have access to a combination of nutritional interventions depending on individual needs, e.g., testing, dietary counselling or oral nutritional supplements
Patients should work with a qualified professional to develop personalised nutrition interventions e.g., calories, macro/micronutrient needs to include vitamin D, protein, and omega-3 fatty acids
Patients should have access to other treatment modalities, e.g., physical activity, exercise and/or psychological support, to help patients achieve the outcomes that matter to them
Patients should be given support to manage loss of taste and smell which can interfere with nutritional optimisation programmes
A focus on key nutrients

Protein
Muscle weakness accompanied with or without muscle loss has been observed for many years in patients hospitalised for severe illness such as and disease. The breakdown of muscle to provide the much-needed protein to help fight infection is one of the causes of weakness and fatigue. A body composition assessment can be performed by healthcare practitioners to assess the degree of muscle loss; and it may be necessary to consume a higher-than-average protein diet to around 1.4g/kg/day post infection to promote muscle repair and regeneration.
Essential fatty acids (EFA’s)
EFA’s represent a group of fats that can only be obtained from the diet. They are commonly referred to as omega 3 and omega 6 fats. Omega 3’s have a propensity for being anti-inflammatory as opposed to Omega 6 which signal both inflammatory and anti-inflammatory pathways. Neither is good or bad, however western diets tend to favour consumption of Omega 6 fats over Omega 3’s. The very special benefits of Omega 3 fats are that they produce immune supporting mediators called Specialised Pro-Resolving Mediators or SPM’s. SPM’s are vital for resolving inflammation and could stimulate the resolution of lung inflammation and reduce tissue damage in patients with Covid-19. In addition, they could be used to decrease chronic inflammation in the post-acute phase. Omega 3 fats can be obtained from grass-fed meat, oily fish, organ meats, grass fed dairy, algae, nuts and seeds.
Vitamin D
A role for vitamin D in the response to Covid-19 infection could be twofold. Firstly, vitamin D supports production of antimicrobial peptides in the lining of the respiratory system, making infection and development symptoms less likely. Secondly, vitamin D might help to reduce the inflammatory response to infection. Emerging research does suggest that vitamin D is helpful for acute phases but studies are yet to conclude whether there is relevance to the reduction in long covid, In any case the best thing to do is routinely check vitamin D levels with a healthcare professional to see if they need correcting with supplementation. Re-testing is important to ensure levels don't go too high with supplementation (6)
B vitamins
B vitamins can modulate immune responses by reducing pro-inflammatory cytokines and inflammation, controlling breathing difficulties, supporting gastrointestinal problems, and preventing hyper coagulation. B vitamins may prove and essential component in supporting recovery from Covid. Below is a list of B vitamins, their functions in the body, and dietary sources.
B Vitamin | Benefits | Food Sources |
B1 (Thiamine) | Supports immune function, energy production cardiovascular and brain health | Peas, Some fresh fruits (such as bananas and oranges), Nuts, Brown/wholegrain Rice, Liver, Trout |
B2 (Riboflavin) | Supports the skin, eyes, nervous system, and energy production | Milk, Plain Yogurt, Eggs Organ meats, Lean meats Green vegetables Mushrooms |
B3 (Niacin) | Supports energy production and acts as a building block for NAD+ which is vital for decreasing chronic inflammation | Meat, Seafood, Milk, Plain Yogurt, Brown rice Peanuts |
B5 (Pantothenic acid) | Decreases inflammation, helps lower cholesterol, and supports brain function and mental health | Chicken, Beef, Liver, Kidneys, Eggs, Mushrooms, Avocado, Oats, Brown Rice |
B6 (Pyridoxal 5′-phosphate, Pyridoxine) | An essential cofactor in various inflammatory pathways. Optimum levels may maintain the integrity of blood vessel lining and prevent blood clotting | Starchy vegetables Poultry, Seafood, Organ Meats, Peanuts, Wheatgerm, Oats, Bananas, Milk |
B7 (Biotin) | Supports hair, skin and nails, helps support blood sugar regulation, nervous system and the thyroid | Beef, Organ meat, Eggs, Wheatgerm, Sunflower Seeds, Sweet Potatoes, Almonds |
B9 (Folate) | Folate may prevent viral replication in the initial stages of infection | Broccoli, Brussels Sprouts Leafy green vegetables, Peas, Chickpeas, Kidney Beans, Liver |
B12 (Cobalamin) | Supports energy production, red blood cells, nervous and cardiovascular system.Acts as a modulator of the gut microbiome | Meat, Seafood, Milk, Cheese, Eggs |
Pre and probiotics
At the start of the pandemic researchers began reporting that Covid-19 patients generally displayed imbalances between friendly and unfriendly bacteria in the gut, called dysbiosis. The Centre for Gut Microbiota Research produced one of the first studies reporting that an individual’s microbiome profile may affect their susceptibility to long-term complications of Covid-19. They also found that a distinct gut bacteria composition at admission to hospital was associated with occurrence of persistent symptoms at 6 months.
It is widely acknowledged that gut plays a major role in the regulation of the immune system, therefore, disturbances in the gut microbiota may not only exacerbate Covid-19 but may also cause lingering symptoms as a result of continuing immune disturbances. (8)
Data from Kings College London also showed a correlation between taking regular probiotic supplementation with a lower risk of catching Covid. Further analysis of a subset of 126 people showed that a 30 day course of a pre and probiotic supplement containing inulin and lactobacillus improved cough, fatigue, gut and well-being scores for early phase and chronic phase infections. (9). Following more clinical trials it is possible that standardised treatment approaches might include diets and supplements that support the gut microbiome of long haulers.
Types of therapeutic diets that have been hypothesised to support long covid

Low-Histamine Diet
As previously mentioned, chronic low grade inflammation may be one of the factors that exacerbate the symptoms of Long Covid. This is partly caused by dysfunctional mast cells which release histamine and other inflammatory signalling cells. Therefore, low-histamine diets may be an appropriate intervention to help alleviate its symptoms. Foods that contain a lot of histamine include canned, fermented, or pickled foods peanuts, tree nuts, oranges, bananas and spinach. At present the British Dietetics Association conclude that not enough evidence is available to support the recommendation of a low histamine diet for long covid, however for those who wish to try our this intervention are best off working alongside a professional who can ensure food intake its meeting requirements.
Anti-inflammatory or Mediterranean style diet
An anti-inflammatory diet may help manage symptoms of long covid by reducing the effects of the inflammatory process. Highly processed or refined foods are the main things to avoid since they have been shown to increase the risk of metabolic disharmony, type 2 diabetes, obesity, and chronic low grade inflammation. Each of these factors contributes to the overall severity of Covid-19 and its long-term symptoms.
The aim of an anti-inflammatory diet focuses on eating whole plant-based foods and animal based products that are not only rich in healthy fats, proteins and carbohydrates, but also phytonutrients. This way of eating can help to balance blood sugar, promote healthy gut function and body composition which are primary targets when supporting those dealing with Long Covid.
Intermittent Fasting
Some animal and human studies have suggested that intermittent fasting regimens may be beneficial for Covid patients, and promote weight loss, healthier body composition, and glucose tolerance. The most traditional method of intermittent fasting is to pick an over night fasting window, which is generally 12, 16, or 18 hours from the last meal of the previous day to the first meal of the next day. The mechanism behind the efficacy of intermittent fasting are beyond the scope of this particular blog post and will be covered in depth later, however this intervention is not recommended for patients who are already underweight and malnourished.
General dietary interventions that are proving beneficial with my clients
The research on the most effective nutritional intervention strategies is still ongoing and will evolve over the next few years. In the meantime it is important that nutrition plans focus on including whole foods, fruits and vegetables; foods that contain phytochemicals and essential fatty acids to support inflammation, the right amount of protein to support recovery, and reduced consumption of processed, sugary and nutrient depleting foods. Individuals managing more serious conditions involving the heart, kidneys, lung or nervous system need to supported professionally to improve outcomes and ensure the diet is optimised to support specific health challenges.

With all of the above in mind, my dietary protocols are uniquely tailored according to each individual and form part of my resistance resilience and recovery programme which focuses on 5 key areas of wellness which will be covered in a future blog post.

REFERENCES
(1) Crook H, Raza S et al., 2021. Long covid—mechanisms, risk factors, and management BMJ 2021; 374,n1648 https://www.bmj.com/content/374/bmj.n1648
(2) NICE., 2022. Covid-19 Rapid guidance: Managing the long-term effects of Covid-19 v1.13 Published 02/01/2022 https://app.magicapp.org/#/guideline/EQpzKn/section/n3vwoL
(3) Asadi-Pooya AA, Akbari A, Emami A, et al. Risk Factors Associated with Long COVID Syndrome: A Retrospective Study. Iran J Med Sci. 2021;46(6):428-436. doi:10.30476/ijms.2021.92080.2326 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8611223/
(4) Cereda E., Clavé P., et al,. 2021. Recovery Focused Nutritional Therapy across the Continuum of Care: Learning from COVID-19. Nutrients 13(9):3293. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8472175/
(5) Fernández-Lázaro D, Sánchez-Serrano N, Mielgo-Ayuso J, García-Hernández JL, González-Bernal JJ, Seco-Calvo J. Long COVID a New Derivative in the Chaos of SARS-CoV-2 Infection: The Emergent Pandemic? J Clin Med. 2021 Dec 11;10(24):5799. doi: 10.3390/jcm10245799. https://pubmed.ncbi.nlm.nih.gov/34945095/
(7) Shakoor H, Feehan J, Mikkelsen K, et al. Be well: A potential role for vitamin B in COVID-19. Maturitas. 2021;144:108-111. doi:10.1016/j.maturitas.2020.08.007 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7428453/
(8) https://gut.bmj.com/content/early/2022/01/05/gutjnl-2021-325989



Comments